Updated COVID-19 Boosters FAQ
For questions specific to your situation, you should ask the healthcare professional who cares for you.
CDC Nowcast showing current variants circulating in the US and the proportion of cases they account for (note that Nowcast estimates from 08/27/2022 on are extrapolations from prior trends).
Context
In September 2022, the CDC and FDA made the historic move to update the COVID-19 vaccine booster doses for the first time. The new vaccines (from Pfizer/BioNTech and Moderna) are bivalent vaccines, meaning they contain 2 antigens. Specifically, they contain a 1:1 ratio of mRNA encoding the ancestral spike protein that has been used throughout the pandemic and an mRNA encoding the spike protein of the BA.4/5 variant (this is actually the same spike protein; the mutations defining BA.4 and BA.5’s spike are the same, but they have mutations outside of the spike protein where they differ). Currently, virtually all cases of COVID-19 in the US (and most of the world) are due to BA.5 subvariants, and BA.4 subvariants to a lesser extent, meaning the vaccine contains what is currently circulating throughout the world. Elsewhere in the world, instead of a BA.4/5 mRNA, a BA.1 mRNA is being used.
How can I locate an updated booster?
CDC’s interim clinical considerations summarizing authorized or approved vaccine products in the US.
In the US, the vaccines.gov website has been updated to allow you to search for the updated boosters. That is likely a reasonable place to start. Sometimes they are available by walk-in, so it’s also worth checking your local pharmacies. For those who cannot make the trip to the pharmacy such as if homebound, in-home vaccination may be an option in some cities. For example, here is a registration for it in New York City.
Who should get the updated boosters?
In the US, those who have completed a primary series of COVID-19 vaccine and are aged 18 or older should receive an updated Moderna COVID-19 booster and those aged 12 and older may receive an updated Pfizer/BioNTech booster, provided it has been at least 2 months since their last dose (but more is okay, and possibly better- see “How long after my last vaccine dose or case of COVID-19 should I wait to get my booster?”). While everyone in this group should get boosters, it is particularly important to get them if you are elderly, reside in a long-term care facility, have multiple comorbidities that put you at heightened risk for severe COVID-19 (including pregnancy), or work or are in contact with those vulnerable individuals.
Currently, there are no updated boosters for either Novavax or Janssen/Johnson & Johnson vaccines.
I had Pfizer for some/all of my prior vaccine doses and now I want Moderna. Can I switch?
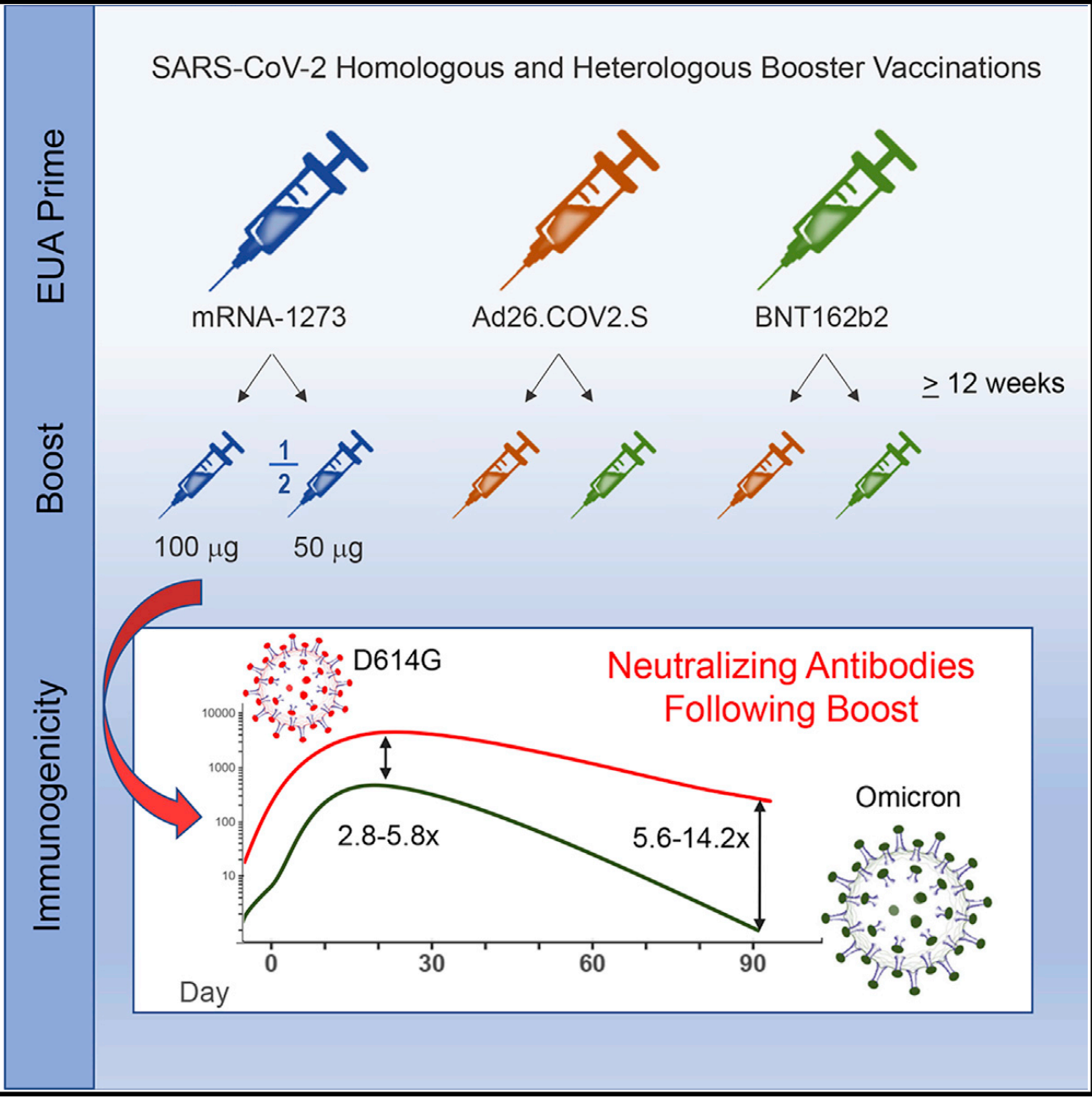
Yes, this is permitted according to the latest recommendations (see: heterologous vaccine booster), provided you are at least 18-years-old (as those under 18 cannot yet receive the Moderna booster). You can also get Pfizer if you have previously received Moderna. It may be relevant to consider though that the side effects with Moderna tend to be a bit more intense than with Pfizer, as was also seen in their clinical trials for their BA.1 boosters. Regarding studies where there is mixing and matching of vaccines, the broad theme of those is that any series that includes an mRNA vaccine does really well as far as the antibody response, but Moderna still seems to give the biggest immune responses overall regardless of what series it’s put in.
How do the Pfizer and Moderna boosters differ? Is one better than the other?
The major difference between the two vaccines is just their dose (they also differ in the specific components of their lipid nanoparticles but the basic types of lipids used are the same). Pfizer’s is 30 micrograms while Moderna’s is 50 micrograms. Moderna also tends to on average give more intense side effects (reactogenicity) than Pfizer, but also seems to outperform Pfizer in the real-world in terms of effectiveness against infections and immunogenicity. It may be worthwhile for younger males (those < 40 years old) to stick with Pfizer given the risk of myocarditis, but in a recent VSD analysis, the risk of myocarditis with the (ancestral) booster dose for males under 50 was similar for both Pfizer and Moderna, possibly because the dose of the Moderna vaccine is lower for the booster dose. An increased risk has not been observed for those younger than 12-years-old with any of the mRNA vaccine doses. Both are excellent options with advantages and disadvantages with neither being clearly better than the other- it just depends on who you are and what characteristics are more important to you. In general though, you should probably take whatever is easier for you to get.
Can I get my flu vaccine at the same time as my COVID-19 vaccine?
You can! Just be aware that there might be more intense side effects if you do both together (not necessarily dangerous- but more discomfort), so you can consider spacing them apart by a few weeks if you prefer to avoid that. Some might also argue that it’s a bit early for the flu vaccine right now (September 15, 2022), depending on who you are.
I’ve heard really great things about Novavax. Can I get that as my booster?
No, Novavax is not currently authorized as a booster for those who have received other vaccines. Novavax may only be used as a primary series in those aged 12 and older who have received no vaccine doses for the time being. Beyond this, several lines of evidence suggest that Novavax does not work very well as a booster to mRNA vaccines (although the reverse does not seem to be true).
When will the booster be available to younger age groups (those younger than 12-years-old)?
In a recent CDC/IDSA clinician call, Peter Marks (head of the FDA’s Center for Biologics Evaluation and Research, CBER) stated that boosters for kids are “several weeks off” and for the youngest (down to 6 months old) it will probably be late fall to early winter 2022-2023. In the meantime though, they need the primary series to be eligible for the bivalent booster. While this is disappointing for many parents for children in those age groups, it’s worth mentioning that Pfizer recently announced in a press release that the original 3-dose series for those aged 5 and younger has shown a vaccine effectiveness of above 70% throughout a period of BA.2 predominance; while this number isn’t quite what we might hope, it’s still quite good considering the vaccines are not matched for Omicron and protection from severe outcomes with the ancestral vaccines remains robust.
I haven’t had the primary series (first 2 doses) of my COVID-19 vaccines yet. Can I get the updated booster?
No (for now). You need to have had at least 2 doses of mRNA vaccine to qualify for the booster; those who received the Janssen/Johnson & Johnson vaccine are recommended to receive an mRNA booster and then a bivalent vaccine at least 2 months after that mRNA booster.
Why are we still using an ancestral spike protein in our bivalent boosters?
The honest answer is because this is what the FDA recommended. I am not privy to the precise thought process underlying that decision; however, Moderna did report during the VRBPAC meeting that the antibody responses it attained with its variant boosters seemed to be consistently better for the bivalent ones than monovalent ones (Pfizer had the opposite result, which is curious). Beyond this, we know that the ancestral vaccine gives excellent protection against pre-Omicron variants, which are still circulating (albeit at very low levels). There is therefore a theoretical risk that in changing the immune landscape of the population to be extra well protected against Omicron, those older variants could come back (as Omicron’s fitness advantage seems to be driven overwhelmingly by its ability to escape antibodies). I think it would have been reasonable to have monovalent BA.1 or BA.4/5 boosters, though.
Why hasn’t the primary series been updated to all be bivalent?
The short answer is: regulation and bureaucracy. While there’s basically no doubt that this would help and it makes sense, there would need to be a lot of additional data generated from the sponsors for the FDA to go through and then for CDC to go through to allow for this. Also I don’t think that supply has been scaled up yet to the point that we can simply replace all the ancestral vaccines in circulation with bivalents.
I am pregnant or lactating- can I get the updated booster?
Yes, and it is recommended that you do. ACOG puts it explicitly:
Anyone age 12 and older who completed an initial COVID-19 primary dose or COVID-19 vaccine series should receive a bivalent booster two months following their last primary dose or monovalent booster.
ACOG recommends that pregnant and recently pregnant people up to 6 weeks postpartum receive a bivalent mRNA COVID-19 vaccine booster dose following the completion of their last COVID-19 primary vaccine dose or monovalent booster.
During pregnancy, the antibodies that circulate throughout your body are transferred across the placenta to provide protection to the baby for the first few months after birth. Booster doses in general are therefore important for increasing the level of circulating antibody and by extension the amount of antibody transferred to the baby; updated boosters will be particularly good for ensuring those antibodies more closely match circulating SARS-CoV-2 strains until the baby is old enough to be vaccinated. A significant decline in protection of infants whose mothers were vaccinated was observed against Omicron (compared with Delta), which reinforces the importance of having the right antibodies.
CDC recommendations for vaccination and Evusheld for those who are moderately or severely immunocompromised.
Regarding lactation, the extent to which human milk is protective against SARS-CoV-2 (and respiratory infections more broadly) is harder to tell, though it certainly will not harm your child. The vaccine also does not end up in breastmilk, so no need to “pump and dump” (though even if it did, the digestive tract of the baby would simply destroy it). A temporary decrease in milk supply has been reported by some after vaccination, however.
In the case of safety, the mRNA vaccines have an extensive record of safety in pregnant and lactating individuals, do not cross the placenta, and do not end up in breastmilk. For details on any matters of the use of the vaccines in pregnant and lactating individuals, I cannot endorse Dr. Victoria Male’s google doc on the subject more.
I am immunocompromised. Can I receive the boosters?
You can and should- mRNA vaccines do not contain or generate any replication-competent virus and thus are safe for immunocompromised people to take. Immunocompromised people may frequently require more doses of a vaccine to generate appropriate responses to them. When to get your booster depends on the reason for your immunocompromised status and which medications you take (ACR has a guide to pausing certain medications to help ensure responses to COVID-19 vaccines here), so speak to the healthcare professional who manages your disease on guidance about that point. Moderately to severely immunocompromised people should also receive Evusheld, a long-lasting monoclonal antibody cocktail against SARS-CoV-2 every 6 months, but allowing for 2 weeks after their last vaccine dose to minimize interference. Please note however that Evusheld is not a substitute for vaccination, and, unfortunately, BA.4.6, a subvariant of Omicron, appears to be capable of escaping Evusheld completely and is increasing in prevalence in the US.
Vaccine effectiveness of Bnt162b2 (the Pfizer/BioNTech vaccine) and Coronavac by number of doses and age. Table 2 from McMenamin ME, Nealon J, Lin Y, Wong JY, Cheung JK, Lau EHY, Wu P, Leung GM, Cowling BJ. Vaccine effectiveness of one, two, and three doses of BNT162b2 and CoronaVac against COVID-19 in Hong Kong: a population-based observational study. Lancet Infect Dis. 2022 Jul 15:S1473-3099(22)00345-0. doi: 10.1016/S1473-3099(22)00345-0. Epub ahead of print. Erratum in: Lancet Infect Dis. 2022 Sep;22(9):e239. PMID: 35850128; PMCID: PMC9286709.
Does the updated booster mean our old vaccines are no longer working?
This question is a bit of a minefield. The short answer is no, although that does depend on what you mean by “working.” Among immunocompetent people (those whose immune systems are not impaired), there is no compelling evidence for waning protection against severe COVID-19 from the ancestral boosters, even against Omicron. Despite this, we see reports all over the place showing shockingly low vaccine effectiveness numbers even against severe disease, so what gives? It’s mainly two things. Firstly: incidental COVID-19. The effectiveness of the vaccines against severe outcomes is much more durable than it is against infection. When looking at effectiveness against hospitalization, assuming it is done simply by comparing the incidence of positive SARS-CoV-2 tests among the vaccinated and unvaccinated within the hospital (and it usually is, plus correction for confounders), it is very likely to find COVID-19 in both groups, wherein for the vaccinees, it is far more frequently not actually the reason they are in the hospital but an accidental discovery. The solution to this is to do chart review to judge whether or not COVID-19 is the reason for hospitalization (ideally blinded to the vaccination status of the patient to not bias their interpretations), and when this is done, the results look quite a bit better. The other reason is something called depletion of susceptibles bias. When you measure vaccine effectiveness, you compare how common an outcome is in your vaccinated vs. your unvaccinated groups. The unstated assumption behind this is only the vaccinated group should have immunity so that you can measure precisely what the benefit of vaccination to protection is, but as more and more of your unvaccinated group gets COVID-19 and recovers from it, they now have immunity too (you could reasonably argue that this doesn’t make the number invalid because it’s reflecting the additional benefit to vaccination in a situation where there is a lot of infection-acquired immunity, but when you’re trying to see how well the vaccine itself does, it makes it a lot harder to understand). Thus, the benefit of the vaccine appears to decline even if it completely unchanged because now the control group is getting more immunity, so the difference in the risk of the outcomes of interest necessarily decreases. When I brought this up initially with some estimates, someone countered with the point that the effects of depletion of susceptibles bias don’t start to really become significant until you hit about 5% of the population infected. Omicron infected half of the US in a matter of 10 weeks and didn’t stop there. Depletion of susceptibles bias here is VERY substantial. If you don’t believe me, consider Hong Kong, which had virtually no infections until their BA.2 wave, and yet even 2 doses of Pfizer had about 90+% vaccine effectiveness depending on the age group (note however that there was a significant benefit to third doses against hospitalizations despite this). There is also the matter of Long COVID, which is a real, serious, debilitating condition. The bulk of evidence suggests vaccines do help to prevent long COVID, but results differ wildly about the extent in large part because there is wide variation in studies regarding what meets the definition of long COVID. Nonetheless, the most definitive way to prevent it is by avoiding infection, which these vaccines will help us to do.
All this to say: the ancestral vaccines continue to hold up very well against severe disease (and this was/is the basis for some reluctance among experts to support an update). They are however lacking in other important outcomes, like infections. The harder it is to prevent infections, the harder it is to prevent transmission, and when that happens, even if the bad outcomes are rare, when you have explosively high levels of infections, they will happen at a rate high enough to put significant stress on the medical system. The main hope is that updated boosters will help to address this deficiency in particular, thereby reducing the frequency and seriousness of everything downstream of infections.
Why are some countries using the BA.1 sequence instead of BA.4/5?
Until relatively recently, to update the COVID-19 vaccines, most regulators required that they be treated essentially like new vaccines where they would need clinical trials in humans to support their authorization. Multiple manufacturers had already made vaccines throughout the pandemic specific to certain variants of concern (for example, Moderna has long had one for the beta variant, but it never submitted it for authorization to the regulatory bodies because this proved unnecessary) and had been testing them throughout. With the emergence of Omicron however, regulatory bodies and manufacturers both felt that it was necessary to have updated vaccines to address Omicron. However, it took 7 months since the emergence of Omicron to conduct the clinical trials in humans necessary to support an updated booster, and this booster was based on the first Omicron subvariant to emerge: BA.1. The FDA, upon considering the evidence for this booster, for what was circulating at the time of the VRBPAC meeting in June 2022, decided to recommend that the updated boosters instead contain BA.4/5 spike and it would allow the vaccines to be approved based on preclinical data, similar to what is done each season for influenza vaccines. Other countries however, maintained the need for human clinical trial data to support any updates. Currently, those are available only for a BA.1 booster, and not a BA.4/5 booster. However, the European Medicines Agency (EMA) has recently announced that it will be purchasing BA.4/5 boosters and will be recommending those for approval as well. BA.4/5 more closely matches what is circulating now, so in that sense may be a better option than BA.1 and we know that BA.4 infections gave significantly broader immune responses than BA.1 infections in South Africa, but this may not directly translate with a vaccine. In short, both boosters are Omicron, and both will help, so you should take whatever is available to you first when enough time has elapsed since your last exposure.
Pfizer’s mouse data supporting the updated BA.4/5 booster.
I heard that the boosters were approved based only on data from 8 mice. Is that true?
No. Pfizer/BioNTech’s updated BA.4/5 booster was approved based on preclinical data, which included a demonstration of the vaccine’s immunogenicity in mice who had received 2 doses of the first-generation vaccine encoding ancestral spike only followed by either BA.1-only boosters, BA.4/5-only boosters, bivalent boosters, or another dose of ancestral booster. The BA.4/5-only booster seemed to give the best responses against Omicron variants overall; the FDA ended up recommending a bivalent booster, seemingly out of an abundance of caution to not give a pre-Omicron variant a fitness advantage in the population (as the ancestral vaccine worked very well against those). Moderna also evaluated the performance of its boosters in a mouse model, and like Pfizer, found them to be superior to the ancestral first-generation vaccine.
However, it is deeply misleading to suggest that this is the only data that went into the booster approvals. Firstly, it’s important to understand that the updated boosters are minor tweaks to existing vaccines and not truly new vaccines per se. Billions of doses of COVID-19 mRNA vaccines have been given around the world and found to have no significant safety concerns (although rarely and mainly in younger males after dose 2, myocarditis has been observed, which is serious but in the vast majority of cases appears to resolve completely on its own/with conservative management, though the long-term consequences of this myocarditis are not yet well defined; this risk appears to be lower for booster doses and for longer intervals between the first and second dose, and higher with Moderna than Pfizer for dose 2). Additionally, clinical trials of the BA.1 boosters were completed and the safety and reactogenicity profile proved to be similar to that of current vaccines. Beyond this, no sudden new hazards of BA.4/5 infections have been observed, reinforcing the safety of the inclusion of their spike protein. This is analogous to the process that goes into updating the flu vaccines each season, which is allowed mainly because we have extensive experience with flu vaccines so we know what to expect from a safety perspective (just like it is here).
The FDA had a complex choice: they could have approved the BA.1 boosters immediately in June/July 2022, knowing that we were past the BA.1 wave (although I would have supported this), or they could have waited to get updated boosters. The issue is: running the clinical trials to get the updated boosters takes time. It took 7 months for the BA.1 boosters, and there’s no reliable way to know what the dominant variants will look like months from now, so putting BA.4/5 through another set of trials taking another 7 months is not reasonable if we want to maximize protection right now (in principle there might be ways to make the clinical trials go faster, but it took 7 months for BA.1, so that’s likely the benchmark). So, the FDA opted to make the reasonable choice of accelerating the release of a BA.4/5 booster- and it is reasonable precisely because we have so much data on this vaccine platform, infections with the relevant variant, and animal models that recapitulate human data on the immune response well, and have throughout the pandemic. I would go as far as saying that people who would attempt to use “8 mice” rhetorically in the manner described in the question don’t have your best interests at heart. As a brilliant friend put it:
Here is a fun fact about research in mice: once you repeatedly show that a biological process behaves similarly in mice and humans, it is in fact ok to trust that mouse data will reflect human data
Still, people should be aware that Pfizer and Moderna are doing the BA.4/5 bivalent vaccines human trials right now anyway because those data are important.
What can I expect after my booster in terms of side effects?
As above, we do not have clinical trial data yet specific to the BA.4/5 boosters, but we do have it for the BA.1 boosters and it was broadly similar to that of the original ancestral spike vaccines given for the booster. You can view those data for Moderna here (slide 8) and for Pfizer here (slide 13). Guidance on managing vaccine reactogenicity (side effects) can be found here.
I think I may have had COVID-19 but I’m not sure. Should I check before I get the booster? Should I even get the booster?
This is an easy one: yes, you should get the booster. There are some nuances here though. If you know a specific time where you may have had COVID-19 but for instance failed to get tested, you might consider asking your primary care physician for an antibody test looking at nucleocapsid (N), a protein from SARS-CoV-2 that is not present in the vaccines and thus can only be acquired by infections (although it is worth noting that in post-vaccine infections, the immune response is sometimes so efficient at clearing the virus that antibodies against N may not have a chance to form at detectable levels). The main reason for this is if you know when you had COVID-19, you can time your booster in a way that maximizes its benefit to your immune system (see next question). If you had an Omicron infection, this booster is potentially especially valuable to you from an immunological perspective. Omicron is very distinct from the variants that preceded it with respect to your antibodies, so to address it, the immune system of vaccinated or people previously infected with pre-Omicron variants will rely primarily on crossreactive antibodies to clear it (this is not a bad thing- people often talk about this like it is a bad thing but it is literally an evolutionary adaptation by the immune system to clear infectious threats as quickly as possible to minimize the amount of damage they get to cause). Getting a booster containing Omicron is an opportunity to boost those crossreactive responses and narrower Omicron-specific responses especially well, which means even better protection from future variants of concern. In other words, it’s like the booster is dose 2 of Omicron (but arguably better because you also have mucosal immunity to Omicron through the infection and we’ve already seen that hybrid immunity with pre-Omicron variants with a single dose of vaccine is significantly more effective than just 2 doses of vaccine). Remember- prior infection due to pre-Omicron was substantially less protective against Omicron infection (although not necessarily severe outcomes) than it was against pre-Omicron variants.
How long after my last vaccine dose or case of COVID-19 should I wait to get my booster?
It depends, but broadly, I think this summary from Dr. Katelyn Jetelina is a useful guide:
Those who were infected about 1 month before their booster doses (12-44 days) had antibody levels at their pre-booster baseline or below by 60 days after the booster, whereas in those with prior infections about 200 days before (orange) and those without prior infections still tended to have significantly elevated antibody levels against all the variants.
Recent SARS-CoV-2 infection abrogates antibody and B-cell responses to booster vaccination
Clarisa M. Buckner, Lela Kardava, Omar El Merhebi, Sandeep R. Narpala, Leonid Serebryannyy, Bob C. Lin, Wei Wang, Xiaozhen Zhang, Felipe Lopes de Assis, Sophie E.M. Kelly, I-Ting Teng, Genevieve E. McCormack, Lauren H. Praiss, Catherine A. Seamon, M. Ali Rai, Heather Kalish, Peter D. Kwong, Michael A. Proschan, Adrian B. McDermott, Anthony S. Fauci, Tae-Wook Chun, Susan Moir
medRxiv 2022.08.30.22279344; doi: https://doi.org/10.1101/2022.08.30.22279344
How much longer to delay should take into account: individual risk (age, comorbidities); degree in which you don’t want to miss an event (because you’re sick) or an event is high risk (wedding, family vacation); and/or not wanting to be sick in general (for example, if someone depends on you). I recommend the following:
<2-3 months since infection/vaccination: Wait.
3-4 months since infection/vaccination: Consider a booster if you’re high risk, or have an event. (Get your booster 2 weeks before this event for optimal protection).
4-6 months since infection/vaccination: Get your booster at some point.
6+ months since infection/vaccination: Get your booster ASAP. This includes me—I haven’t been infected, and I had my booster last November.
The reason for the waiting period is to maximize the benefit of the booster to your immune system. If you have just been vaccinated or infected, your antibodies are still very high and will likely protect you from infection quite well so there’s no point. Beyond this, high levels of antibodies seem to suppress production of the antigen encoded by mRNA vaccines, blunting the response to the booster doses, and it looks like resting B cells are critical to the immune response to the booster, and it takes some time for B cells to return to resting state after a booster or infection. A shorter interval booster will not hurt your immunity generally speaking (at worst it looks like there was a short-lived “extrafollicular response” where there was a temporary burst of antibodies that rapidly faded without conversion to longer lived antibody-secreting cells), but for someone with a normally functioning immune system who is otherwise healthy, getting it 2 months after either infection or a prior vaccine dose is probably not the best use of resources. It is also useful to know that currently, a peak in COVID is modeled for late November 2022, but this could change.
Key point from this figure: antibody titers rise much more rapidly after dose 2 than with dose 1, starting as quickly as between days 2 and 3 after the second dose for the Pfizer/BioNTech vaccine. Note though that these are antibodies that bind spike, not necessarily those that neutralize it.
Ibarrondo FJ, Hofmann C, Fulcher JA, Goodman-Meza D, Mu W, Hausner MA, Ali A, Balamurugan A, Taus E, Elliott J, Krogstad P, Tobin NH, Ferbas KG, Kitchen SG, Aldrovandi GM, Rimoin AW, Yang OO. Primary, Recall, and Decay Kinetics of SARS-CoV-2 Vaccine Antibody Responses. ACS Nano. 2021 Jun 23. doi: 10.1021/acsnano.1c03972. Epub ahead of print. PMID: 34159781.
When does my booster “kick in”?
2-3 weeks after the booster dose is likely the peak of protection; even though the recall response is much more rapid than this, because it is the first time (in at least some cases) that your immune system is seeing the BA.4/5 spike, it is likely best to give it a little bit of time to develop those responses, though the recall responses to Omicron cross-reactive cells will probably show up sooner. Basically, if you need to do something that puts you at high risk for contracting COVID-19, it would probably be in your best interest to get boosted 2-3 weeks before.
Will I need 2 doses of the booster for it to work?
Currently, people can only receive a single dose of the bivalent booster vaccine under the EUA. Whether or not a second dose will be needed for most people is not entirely clear (and again, it depends on what is meant by “need”- for what function: infection, transmission, severe disease, death, or Long COVID?). In people who have not had Omicron, the Omicron component is similar to a first dose of vaccine, which has generally not been enough to robustly protect from infections against pre-Omicron variants. However, in this case, there is also a large base of immunity from the ancestral spike that can crossreact with Omicron that will be recalled by the vaccines; the extent to which this will on its own be enough to prevent cases and their downstream consequences is not entirely clear right now. With so many people having had Omicron though, it is likely that dose 1 is functionally similar to dose 2 for them (although based on how hybrid immunity has worked in the past, after infection, responses peaked after a single dose of vaccine, so perhaps in this situation dose 2 is redundant), so this should not be a major concern. Policy can be adjusted to allow for second doses down the line if it proves necessary.
How can an Omicron vaccine work to give protection against Omicron if Omicron infection doesn’t?
Omicron infection is definitively protective against reinfection by Omicron. I have heard this claim recycled a lot and have no idea where it came from but we have a lot of strong evidence from multiple countries showing quite clearly that it is false and Omicron infection protects from Omicron reinfection (although the time frame for which this holds is not well-defined):
BA.1 or BA.2 infection in Portugal was found to be 75.3% effective at preventing BA.4/5 infection; note however that this is in the context of a population in which 98% of people have been vaccinated.
In Denmark, BA.1 or BA.2 infection was estimated to confer 93.6 (92.1; 94.8)% protection against BA.4/5 infection, but again, in the context of a highly vaccinated population.
In Qatar, it was found that the effectiveness of a previous Omicron infection against symptomatic BA.4/BA.5 reinfection was 76.1% (95% CI: 54.9-87.3%), and against any BA.4/BA.5 reinfection was 79.7% (95% CI: 74.3-83.9%).
The major limitation here is that the analyses are over fairly short periods of time, so we don’t know how durably Omicron protects against Omicron. Nonetheless, there is no reason that an Omicron vaccine should not work to protect against Omicron given that Omicron infection clearly does, and given that it boosts the protection conferred by surviving Omicron, it should reliably extend the duration of protection.
What is imprinting and do I need to worry about it for my booster?
Antigenic maps showing the relative distance of different variants from one another based on the number of vaccine doses and immune history. BA.4/5 and BA.1 are both very far from the D614G ancestral variant, meaning the risk of imprinting is reduced. Source
Post-vaccination Omicron infections induce broader immunity across antigenic space than prototype mRNA COVID-19 booster vaccination or primary infection
Wei Wang, Sabrina Lusvarghi, Rahul Subramanian, Nusrat J. Epsi, Richard Wang, Emilie Goguet, Anthony C Fries, Fernando Echegaray, Russell Vassell, Si’Ana Coggins, Stephanie A. Richard, David A. Lindholm, Katrin Mende, Evan Ewers, Derek Larson, Rhonda E. Colombo, Christopher Colombo, Janet O. Joseph, Julia Rozman, Alfred Smith, Tahaniyat Lalani, Catherine Berjohn, Ryan Maves, Milissa Jones, Rupal Mody, Nikhil Huprikar, Jeffrey Livezey, David Saunders, Monique Hollis-Perry, Gregory Wang, Anuradha Ganesan, Mark P. Simons, Christopher C. Broder, David Tribble, Eric D. Laing, Brian Agan, Timothy H. Burgess, Edward Mitre, Simon D. Pollett, Leah C. Katzelnick, Carol D. Weiss
bioRxiv 2022.07.05.498883; doi: https://doi.org/10.1101/2022.07.05.498883
Imprinting refers to the ability of the first encounter we have against an antigen to leave an “imprint” in our immune response so that when we encounter similar antigens we will deal with them by recalling responses to that first antigen. In this case, the concern is that imprinting will undermine the response to the booster because the ancestral spike protein has left an “imprint” on our immune system that will prevent effective responses against Omicron. You may have also heard the term “original antigenic sin,” to describe this (although there are subtle differences and inconsistencies in the terminology that I won’t get into here). However, as originally formulated by Thomas Francis, original antigenic sin described specifically that children tended to mount better responses against influenza strains they had encountered earlier in life rather than the way it is often used to imply that your responses against antigens different from the first one you encounter are irreparably harmed. I am currently working on a post going through the details of the immunology of how this works but here’s what I will say about it briefly: the extent to which imprinting occurs is a function of the antigenic distance between the original antigen and the target antigen (meaning the better the new antigen escapes antibodies against the old antigen, the less of a problem this is). BA.4/5 is very far from the ancestral spike on antigenic cartography, as is BA.1 (meaning very few of the antibodies that bind to spike also bind to BA.1 or BA.4/5) and so the potential for any kind of imprinting is greatly reduced on that basis alone. However, BA.4/5 spike (or BA.1 spike) effectively functions as bait that pulls out the Omicron crossreactive responses by selecting those memory cells that can respond to both- which is not a bad thing. Furthermore, mRNA vaccines are uniquely well suited to address imprinting (so are adenovirus vectors but they don’t do as good a job boosting the antibody or B cell response) because spike protein is not made until they get inside a cell, at which point they start churning it out. Protein vaccines on the other hand struggle with it more because they can be captured by circulating antibodies immediately, functionally lowering the dose of the vaccine and reducing the boost response. We already have data in humans showing that the antibody response to the updated BA.1 boosters is superior to that of the ancestral vaccines, and animal data showing the response to BA.4/5 boosters is superior than to ancestral boosters. In short, while imprinting is theoretically a concern that we will need to monitor and there are specific situations where it could present a problem, this does not appear to be one of them. You are better off, in general, getting your booster than not getting it, regardless of any imprinting.
Mice given the booster on the same side (ipsi) had significantly higher avidity IgG (meaning it bound the antigen more tightly) than those given the booster on the opposite side (figure D).
Source
Kuraoka M, Yeh CH, Bajic G, Kotaki R, Song S, Windsor I, Harrison SC, Kelsoe G. Recall of B cell memory depends on relative locations of prime and boost immunization. Sci Immunol. 2022 May 6;7(71):eabn5311. doi: 10.1126/sciimmunol.abn5311. Epub 2022 May 6. PMID: 35522723; PMCID: PMC9169233.
Where should I get my booster?
There is no official recommendation regarding this question, but it was provoked by a study in mice looking at influenza vaccination (you can read the conversations with immunologists I had about this here). The effect is likely not huge (so if you don’t remember where your previous doses were or you switched arms or something, don’t worry about it; people tend to get their vaccines in their non-dominant arm so that their activities aren’t as hindered by arm soreness if and when it occurs) but there are some data suggesting that it might be best to get your booster in the same arm as the one you have gotten your previous COVID-19 vaccines in. The reasoning here is that memory B cells from the prior doses seem to like to hang around in the lymph nodes that they are first activated in, so getting the vaccine in the same spot may do a better job of recruiting Omicron crossreactive cells than a different arm, whereas getting it in a different arm might do a better job of getting naive B cells and antibodies specific to just Omicron. However, by virtue of the fact that they are memory cells, anything they do will be much larger than what naive cells being stimulated for the first time do, hence the preference some expressed for the same arm. In the mice, the overall antibody response was similar regardless of which side the booster was done on, but the antibodies themselves that were elicited by the booster were much more potent when they were given on the same side.
Anyway, if you’re not sure which arm you got it in or for some reason want it in a different arm, or not in your arm I guess, that’s probably fine too- this is mostly academic right now.
Omicron neutralizing antibody titer declines much more quickly than the overall neutralizing titer against ancestral spike when ancestral spike vaccines are used, even though the peak titer is actually not bad. Source
Lyke KE, Atmar RL, Islas CD, Posavad CM, Szydlo D, Paul Chourdhury R, Deming ME, Eaton A, Jackson LA, Branche AR, El Sahly HM, Rostad CA, Martin JM, Johnston C, Rupp RE, Mulligan MJ, Brady RC, Frenck RW Jr, Bäcker M, Kottkamp AC, Babu TM, Rajakumar K, Edupuganti S, Dobrzynski D, Coler RN, Archer JI, Crandon S, Zemanek JA, Brown ER, Neuzil KM, Stephens DS, Post DJ, Nayak SU, Suthar MS, Roberts PC, Beigel JH, Montefiori DC; DMID 21-0012 Study Group. Rapid decline in vaccine-boosted neutralizing antibodies against SARS-CoV-2 Omicron variant. Cell Rep Med. 2022 Jul 19;3(7):100679. doi: 10.1016/j.xcrm.2022.100679. Epub 2022 Jun 20. PMID: 35798000; PMCID: PMC9212999.
How well do these updated boosters work?
Omicron-neutralizing titers in response to a BA.1 booster (mRNA-1273.214) from Moderna in humans. A key point here: at this point, the response that is most representative of what is happening in the population is actually the seropositive group’s given how many people have been infected with SARS-CoV-2. Note that for seropositive individuals, the difference in antibody titer at day 29 is about 2-fold when comparing the BA.1 booster vs. the ancestral, but it’s about 1.65-fold when looking at the seronegative group.
I should preface this by saying that given the massive depletion of susceptibles bias I mentioned earlier and the fact that Omicron is itself much faster (in terms of how it replicates) than older variants, it is unlikely that we will be able to restore the 95% protection from symptomatic infections we saw in the original Phase 3 clinical trials for mRNA vaccines. This is a tough question to answer rigorously though, because, as I said earlier, BA.4/5 boosters were approved based on preclinical data, so I can’t give you numbers for effectiveness or efficacy. We can say with a good degree of confidence that they will work better than the ancestral boosters if only because they induce higher levels of antibodies to them (though how much better is an open question). A preprint modeled that effect here, showing a benefit, though it was small. I think though there are some issues with this analysis, the major one being: protection over time. The models we have where you input an antibody titer to compute some level of protection work quite well (provided you have appropriate convalescent samples to use as a control) but they can only tell you the level of protection at a given moment in time. It is not surprising that a 1.5-fold higher peak antibody titer does not have crazy benefits to vaccine effectiveness (especially when vaccine effectiveness starts out very high), but there is the matter of how long that titer can be maintained. In the course of your antibody response to the spike protein, you make many antibodies that work quite well against many variants, including those that might not exist yet (like Omicron in the pre-Omicron era). The issue is: the immune system has no way to know that the antibodies that are good against Omicron are the ones it should keep around if it has never seen Omicron. That means that the antibodies that work well against Omicron decline much more rapidly than those against the ancestral spike protein, and we see that with that decline, though initially a booster does a fairly good job of boosting protection against infection by Omicron (3 doses of Pfizer were about 70% effective against mild-to-moderate BA.2 symptomatic infections via Hong Kong data above), that protection wanes rapidly. But, when the match is better, the antibodies decline more slowly. For example, Moderna has a Beta variant booster which has key substitution at position 484 on the spike protein that Omicron also has substitutions in (and is responsible for a ton of antibody escape), and antibody titers against both Beta and Omicron decline much more slowly. It stands to reason that the results for an even better matched booster will decline even more slowly. If that were it, I would say that the boosters are unlikely to give a game-changing level of protection but they will help and are worth getting on that basis alone- but there’s more to it than that. In the US, we had a staggeringly high number of Omicron infections- by April 2022, it was estimated that 60% of the US had been infected, and that number has only gone up. This means that there is a lot of potential Omicron-specific immunity in the population to exploit for hybrid immunity, which to date represents the highest level of protection against COVID-19. To be clear, I am not encouraging that people get infected by SARS-CoV-2 and would never encourage it (what on earth is the point of getting infected to avoid getting infected?), but insofar as it happened that so many people were infected, why would we NOT take advantage of that to maximize our protection against future variants? For one thing, this has the basic effect of essentially turning dose 1 of an Omicron vaccine into dose 2, with resultant enhanced responses to Omicron. Antibodies among those who had prior COVID-19 and receive boosters are much higher and decline more slowly, and on that basis alone would be expected to confer better protection. However, there are also data supporting that mRNA vaccination after infection boosts mucosal immunity with T cells homing to the respiratory tract after vaccination in those who recovered and antibodies, including secretory IgA (although there are some contradicting data on this point, I think in part explainable in the linked study by the high proportion of those receiving Oxford/AZ’s vaccine), against variants. Taken together, I would argue that if booster uptake is high, especially among those who have recovered from Omicron infections, these boosters could put us in an excellent position against COVID-19 (and future variants of SARS-CoV-2) on all levels: cases, transmission, hospitalization, ICU admission, and death (although on the latter 3, the ancestral vaccine alone seems to have us covered). The issue is: the effectiveness of a vaccine not taken is 0%, so be sure to get yours when your time comes around.
Won’t some new subvariant of Omicron or a new variant altogether just show up at some point, though?
This is a fair question. The answer is almost certainly yes- eventually. The thing is: we do not need a perfect match. The ancestral vaccines worked very well against pre-Omicron variants including alpha, beta, and delta, even though they were not designed to address those variants. The same will be true here: Omicron is constantly spawning new subvariants and these all have slightly different properties with respect to antibody escape, and that will happen because that is what viruses do. The ones that have the potential to escape neutralizing antibodies are the ones that have a chance to infect other people and get passed on. However, as our immunity becomes diversified against different variants, they end up with increasingly fewer escape routes. Omicron was fairly anomalous in that it had accumulated an unusually high number of spike mutations, many of which are on their own deleterious but together manage to compensate for one another, and likely evolved in a chronically infected, immunocompromised host (and I’d wager one who had been receiving convalescent plasma). It is not typically the case that variants make a rapid mutation jump like that, but it happened. However, now any variants that emerge will have to deal with antibodies that potently neutralize the ancestral spike, and BA.4/5 or BA.1 and anything caught in between (in a universe where we have high uptake of the updated boosters)- which is a lot harder for them to do than if it’s just BA.1 or BA.4/5 or ancestral. Beyond this, we know there are antibodies out there that broadly neutralize betacoronaviruses (the genus of viruses that SARS-CoV-2 and SARS-CoV-1 belong to), and with continued diversification of the immune response, we are increasingly likely to produce them. In other words: yes, eventually, some variant will probably emerge to escape the protection from infection that this vaccine confers- but that doesn’t mean we should forgo the added protection it offers now. We can always update them again if that becomes necessary, as we do each season for flu.